Osteoarthritis is a chronic degenerative disease that affects all parts of the joint: cartilage, articular membrane, ligaments, capsule, periarticular bones and periarticular muscles and ligaments.
According to European doctors, arthrosis accounts for almost 70% of all rheumatological diseases. People aged 40-60 years are more susceptible to joint arthrosis. This is facilitated by both lack of movement and prolonged overload, poor nutrition and, of course, injuries.
What is a node?
Typically, a human joint consists of 2 or more connecting bones. All working surfaces of the joint have a protective coating and are constantly lubricated with synovial fluid for better gliding. The joint cavity itself is hermetically sealed by the articular capsule.
In our body, there are many joints that are "responsible" for certain types of movements, can experience different loads and have different safety limits.
The amount of motion at the joint depends on the structure of the joint, the ligamentous apparatus that limits and strengthens the joint, and the various muscles attached to the bones by tendons.
Causes of joint arthrosis
Normal joint functioning is possible with continuous self-renewal of cartilage tissue. At a young age, the rate of death of old joint cells is equal to the rate of birth of new cells. Over the years, the process of cell renewal slows down and cartilage tissue begins to thin. The production of synovial fluid also decreases. As a result, the articular cartilage begins to thin and break down, leading to osteoarthritis.
In addition, there are other causes of joint arthrosis:
- increasing physical activity. Arthrosis of the joints is a frequent companion of excess weight. As a result of the overload, microtraumas are created in the joints. Athletes develop joint injuries due to increased loads on "unheated" joints;
- joint injuries;
- congenital or acquired deformities of the musculoskeletal system (rickets, kyphosis, scoliosis, improper fusion of bones after injuries with the appearance of limb deformities: O and X-shaped deformity of the legs).
Stages of arthrosis
Depending on the degree of cartilage tissue destruction, different stages or degrees of arthrosis can be distinguished.
Degrees and symptoms of arthrosis
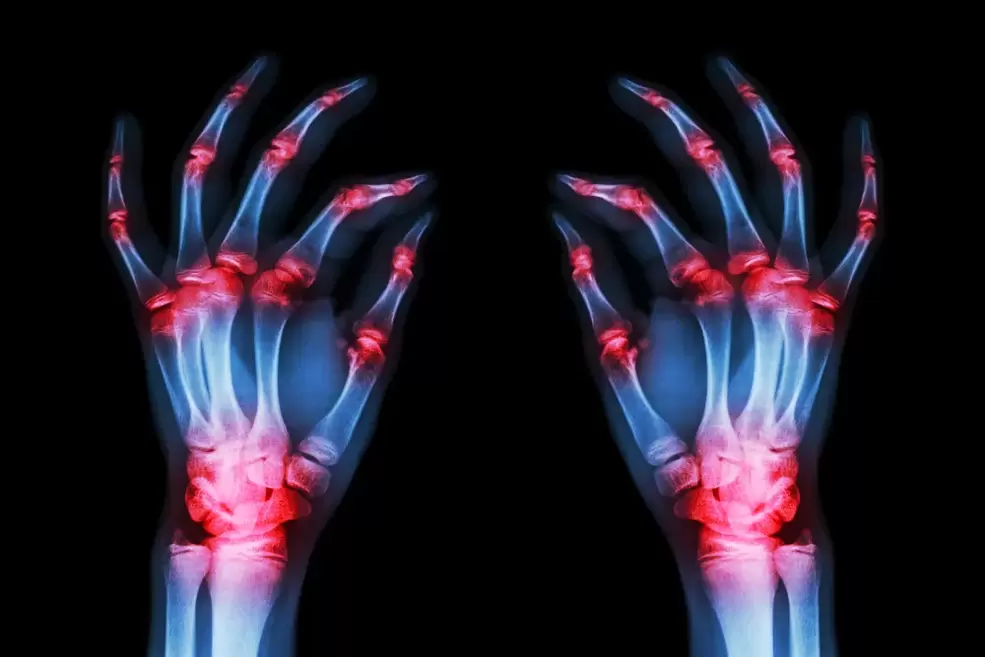
- First-degree arthrosis is characterized by periodic pain in the joints, especially with increased physical activity. After rest, the pain usually disappears. The range of motion in the joint is not limited, the strength of the muscles in the injured limb does not change. X-rays may show minimal signs of joint damage.
- Arthrosis of the 2nd degree is manifested by painful sensations not only with strong physical stress, but also with small loads. Even during rest, joint pain cannot go away. This degree is characterized by stiffness in movement and limited joint mobility. This eventually leads to muscle atrophy. An x-ray may show joint deformity, a decrease in the joint space, and the appearance of bony growths near this space.
- Arthritis of the 3rd degree - every movement causes a person great pain. Joint pain is present even at rest. Therefore, a person tries to move as little as possible so that the pain is minimal. In some cases, mobility requires the use of crutches or a gurney. Sometimes bone fusion occurs - ankylosis (as in ankylosing spondylitis).
With deforming arthrosis, irreversible changes occur in the cartilage tissue of the joint and its functions and structure are completely destroyed. Deformative arthrosis of the joints is based on the occurrence of dysfunction in the formation of hyaline cartilage and synovial fluid.
Diagnosis of joint arthrosis
The main method for diagnosing joints is radiography. With arthrosis, joint changes, uneven joint surfaces and joint space narrowing can be observed.
Which joints are most likely to suffer from arthrosis?
The joints of the extremities most susceptible to arthrosis are the hips, knees, shoulders, elbows and hands.
With arthrosis of the hip joint, a person may initially feel slight discomfort in the leg after running or walking. Over time, pain intensifies, limitation and stiffness in movement appear. With stage 3 disease, the patient protects his foot and tries, if possible, not to step on it.
Osteoarthritis of the knee joint manifests itself as pain in the knee joint after bending and straightening the legs. The most common cause of knee arthrosis is past injuries. As a result of these damages, the gliding of the articular surfaces is disrupted and their rapid wear occurs. In some cases, the joint may gradually lose its mobility.
Ankle arthrosis manifests itself in the form of swelling and pain in the ankle. The cause of arthrosis of the ankle joint can be: deformities, fractures of the ankles and limbs, dislocations, flat feet, chronic injuries of the ankle joint in athletes and ballerinas. By the way, they often have foot arthrosis.
Osteoarthritis of the shoulder, elbow and wrist joints most often occurs as a result of injuries, bruises, dislocations and intra-articular fractures. Osteoarthritis of the shoulder joint is characterized by severe, aching, dull pain that radiates to the forearm and hand. The pain most often occurs at night. With arthrosis of the hands, the pain is accompanied by dysfunction of the hand.
Treatment of arthrosis
The main means of treating arthrosis are drug treatment, the use of physiotherapy and surgical treatment.
Drug treatment
The use of medications helps improve blood circulation in damaged joints, restore cartilage properties, and has an analgesic and anti-inflammatory effect.
Nonsteroidal anti-inflammatory drugs
With arthrosis, swelling of the joint may occur, the joint begins to hurt, and the range of motion decreases. When you take anti-inflammatory drugs (NSAIDs), the pain decreases, the inflammatory chain reaction is interrupted and the cartilage restoration process is accelerated.
Medicines can be used in the form of tablets, rectal suppositories and powder. But remember that self-medication is unacceptable; the selection and dosage of medication for arthrosis is carried out by a rheumatologist.
Centrally acting pain reliever
Opioid drugs lower the patient's pain threshold. Such medications can be taken strictly according to the prescription and only under the supervision of a doctor!
Condoprotective medications
Chondroprotective drugs are structural elements of the cartilage itself, therefore they actively restore this tissue and prevent its further destruction. The treatment is effective in the initial stages of the disease. When the joint is already completely destroyed, it is not possible to return the original shape of the deformed bones or to grow new cartilage.
However, in stages 1-2 of arthrosis, chondroprotectors can bring considerable relief to the patient. Combined preparations, which include both glucosamine and chondroitin sulfate, give better results compared to a single-ingredient preparation.
Chondroitin sulfate and glucosamine sulfate
These medications help slow the inflammatory response in the tissue, help reduce cartilage damage, and reduce pain. Most often, these 2 drugs are used together in treatment, as they have an accumulative effect, but they must be taken for 3-6 months.
Hyaluronic acid
Provides viscosity and elasticity of synovial fluid. It helps the joints slide well. Therefore, doctors often prescribe injections of hyaluronic acid in the affected joint.
Physiotherapy treatments
Physiotherapy treatments may include:
- UHF therapy;
- magnetic therapy;
- low intensity laser radiation;
- electrophoresis with drugs;
- phonophoresis (using ultrasound to introduce a drug to the site of inflammation).
Surgery
Surgical treatment is used to restore and improve joint mobility, as well as to remove part of the damaged cartilage or meniscus.
Surgical treatment of arthrosis is used in extreme cases, when drug treatment does not give results, when there is severe pain, partial or complete immobility in the joint.
During arthroscopic surgery, it is possible to remove part of the cartilage affected by arthrosis, polish it to give a smooth surface, remove cartilage fragments and growths, and cut part of the damaged ligaments.
Knee replacement
With this operation, the articular surfaces of the knee joint are replaced with metal or combined prostheses. The prepared plates replicate the surface of the articular cartilage. Such prostheses are made of special compounds, they do not cause a rejection reaction in patients, do not oxidize and do not damage the surrounding tissues.
Hip surgery for arthrosis
During this operation, the partial removal of the cartilage and bone tissue of the pelvis and femur is performed. Typically, the femoral head and the articular surface of the pelvic bone are removed and replaced with a metal or metal-ceramic prosthesis.
Diet for arthrosis
Excess body weight is a great enemy of your joints. Most patients suffering from arthrosis of the hip and knee joints are overweight.
Therefore, a properly selected diet is recommended for arthrosis. It is believed that jellied meat cooked in cartilage juice is beneficial for arthrosis. It contains a lot of collagen and structural components of cartilage, which help restore cartilage tissue.
Dairy products, protein and calcium are helpful. Animal protein is found in lean meat and fish, while plant protein is found in buckwheat porridge, beans and lentils. Boiled, boiled and steamed dishes are very healthy.
The best diet for joints is a diet with a slight predominance of carbohydrates (preferably complex carbohydrates), fruits and vegetables and a sufficient amount of protein and calcium.
Prevention of arthrosis
Prevention of arthrosis, no matter how trivial, lies in a healthy lifestyle. If possible, try to be in the fresh air, move, walk barefoot on sand, green grass and only on the ground. This type of walking improves muscle function and increases blood circulation in the legs.
Using physical therapy with various arm and leg swings, twists and turns will provide potential support for your joints.
Patients often ask if alternative treatment for arthrosis is possible? Yes, folk remedies can help in the initial stages of the disease, reduce pain and improve the general condition of the patient. But it does not replace following your doctor's instructions.



































